
What is VRI?
Vibration response imaging (VRI) is a noninvasive radiation-free continuous lung imaging systyem that records lung sounds from sensors applied to the patient’s back. TheVRIxp device records the vibration response generated by lung sounds and converts the data into dynamic lung images.
PRODUCTS

What is expected during the procedure?
- One set of V-Array sensors are places on the patient’s back
- The patient breathes normally for twelve seconds
- Results are displayed immediately on-screen
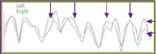
Healthy
- Right & left lung vibration areas similar in size & sharp
- Vertical & bilateral movement of vibration energy
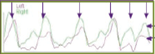
COPD – Smokers
- Narrowing & diffused uneven distribution of vibration energy areas as opposed to the normal image – “Disco Lungs”
- Difficult to delineate between inspiration & expiration with the vibration energy grahg
Asthma
- Unequal expansion of vibration energy area
- Asynchrony in the movement of vibration energy present for both lungs
- Abnormal pattern in the vibration energy graph
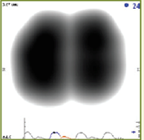
CHF
- Bilateral norrowing of vibration energy areas in both lunga
- Tear-drop shaped lungs due to presence of fluid in the lower part of the lung areas
CHF vs. COPD in the ED…A Critical Choice
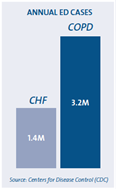
- Over 4.5 million patients present to the ED with CHF and COPD each year
- Differentiating the origin of dyspnea as CHF or COPD is often difficult:
- Physical exam findings, lab tests such as BNP, and chest radiographs can be nonspecificRapidly and accurately determining the cause of dyspnea;
- Is extremely important in proper patient management
- Improves throughput and reduces cost
Know the Difference.
Selecting the optimal treatment path makes all the difference.
- Bronchodilator therapy may have a worsening impact on cardiac function in patients with CHF
- Diuretics may have a worsening impact on COPD patients who are already fluid depleted
Differentiate. Treat. Manage.
VRIxp aids in diagnosis, monitoring and patient management.
- Identifies characteristics that assist in differentiating between CHF and COPD:
- In a study of patients with confirmed diagnosis of CHF and COPD VRIxp was superior to published data for clinical judgment and comparable to CXR and the performance of BNP in the Breathing Not Properly Trial1.
- Three main VRIxp acoustic findings help differentiate COPD from other conditions; heterogeneity, vibration energy distribution differences between inspiration and exhalation and a significantly longer exhalation phase2.
- During acute CHF exacerbations, VRIxp shows more homogeneity in patients after clinical improvement3.
- Contributes to the process of differential diagnosis quickly, and at the point of care
- Serial measurements of patients to indicate treatment progress
CHF Pre-Treatment

Reduction of breath sounds in the bases Dynamic disturbance seen in both lungs
(Courtesy of B. Wiederhold, MD; Highland General Hospital, Oakland, CA)
COPD Pre-Treatment

Dynamic disturbance seen in both lungs
(Courtesy of K. Guntupalli, MD; Ben Taub Hospital, Houston, TX)
- Using VRI Lung Sound Measurements to Differentiate between COPD and CHF in the Emergency Department [Abstract]. Presented at the 2010 Western Regional SAEM Meeting.
- Wang Z, et al. Lung Sound Analysis in the Diagnosis of Obstructive Airway Disease. Respiration. 2009;77(2):134-8.
- Wang Z, et al. Respiratory sound energy and its distribution patterns following clinical improvement of congestive heart failure: a pilot study. BMC Emerg Med. 2010 Jan 15;10(1):1.
Asthma Management in the ED
- There are approximately 1.8 million adult ED visits for acute asthma each year; a significant percentage are uninsured
- Objective measures of obstruction and response to treatment in the ED are currently limited to peak flow and volume measurements:
- Both are dependent on patient effort
- Both can induce bronchospasms
- Better disposition decisions may reduce ED bounce-back rates, reducing costs
Easy. Objective. Rapid. Reproducible.
Because you want to make the right disposition decision…the first time.
- Easy, non-effort dependent procedure eliminates patient variability with current methods
- Objective measure of airway obstruction provides a more precise clinical picture of asthma exacerbations
- Rapid, functional assessment of bronchodilator response saves valuable time and reduces the probability of bounce-backs
- Reproducible look at regional lung function over time means decision confidence from ED admission to discharge
The New Multi-tasker.
VRIxp aids in diagnosis, monitoring and patient management.
- Asynchronous breath sounds between the lungs during acute exacerbations of asthma:
- VRIxp shows significantly higher levels of inspiratory and expiratory asynchrony between right and left lungs in asthmatic patients compared to non-asthmatic patients4.
- Respiratory acoustic analysis demonstrated significant asynchrony between right and left lungs during asthma exacerbations, which was significantly reduced following treatment5.
- Automatic identification of lung sounds consistent with wheezes
- Serial measurements of patients to indicate treatment progress
VRIxp images before and after bronchodilator treatment
Admission

FEV1 84%
Wheezes (red dots) indicated in upper left lung
Asynchrony of breath cycles between right and left lungs
Follow-up Post-1st Dosage of BD

FEV1 95%
Wheezes indicated throughout right lung
Asynchrony improved
DISCHARGE Post-2nd Dosage of BD
FEV1 102%
No wheezes indicated
No asynchrony
(Courtesy of Z. Wang, MD; Cooper University Hospital, Camden, NJ )
4. Pollack, Charlie, et al. Comparison of VRI Patterns in Acute Asthmatic Patients and Non-asthmatic Patients in the ED [Abstract]. Presented at the 2010 National
SAEM (Phoenix) and Western Regional SAEM (Sonoma) Meetings.
5. Wang Z, et al. Asynchrony between left and right lungs in acute asthma. J Asthma. 2008 Sep;45(7):575-8.

